
Pressure sores often develop gradually and may not be immediately visible, particularly in care settings where individuals are unable to move independently or communicate discomfort. Understanding how they form helps explain why prevention must be proactive rather than reactive.
In many situations, pressure sores are not caused by a single event. Instead, they develop when early warning signs are missed or when preventative care measures are applied inconsistently.
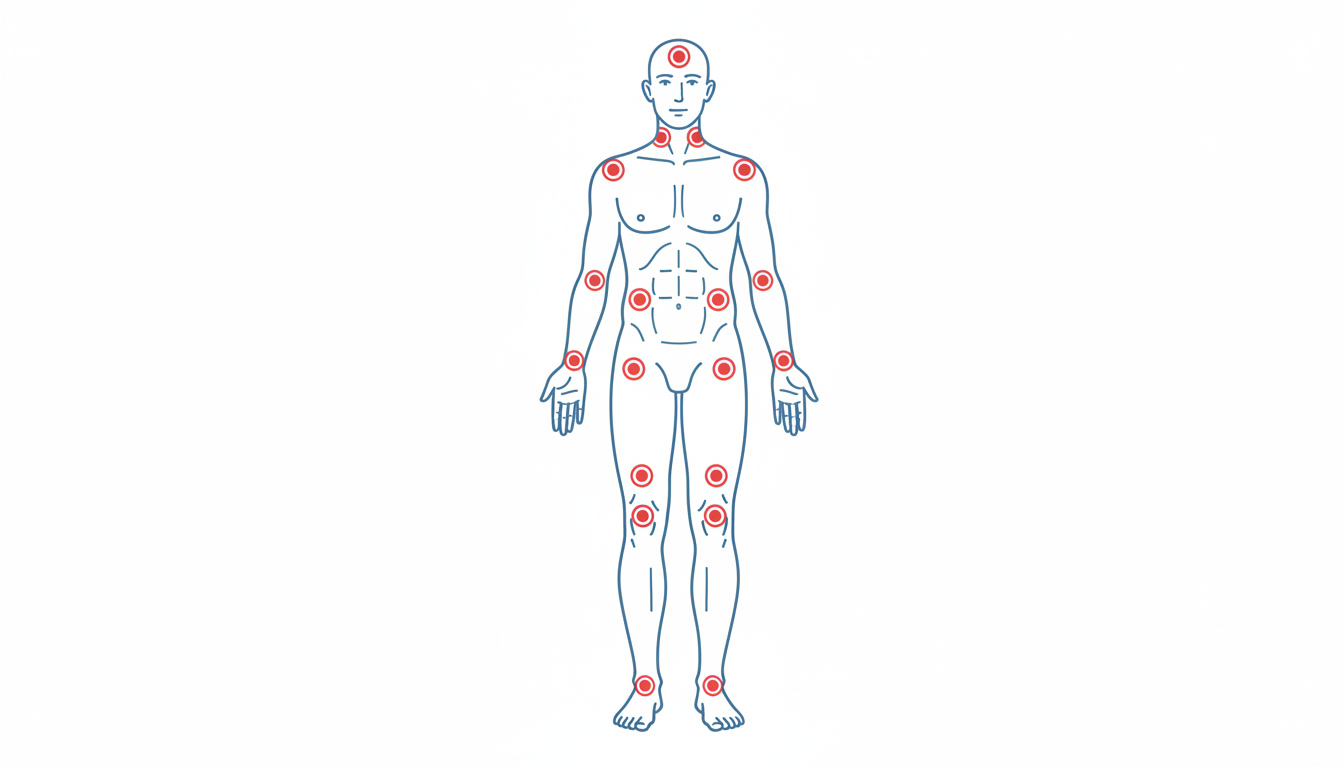
Early signs of pressure damage
The earliest signs of pressure damage can appear within hours of sustained pressure. These may include persistent redness, warmth, swelling, or changes in skin colour that do not fade when pressure is relieved.
At this stage, the skin may still be intact, but underlying tissue damage may already be developing. Prompt action at this point can often prevent further deterioration.
Common contributing factors in care settings
Several factors commonly contribute to pressure sore development in care environments. These factors often overlap and can compound risk if not managed together.
- Infrequent or inconsistent repositioning
- Inadequate pressure relieving equipment
- Moisture from incontinence or perspiration
- Poor nutritional intake or dehydration
- Unclear or outdated care plans
Why prevention matters
Preventing pressure sores is both a clinical responsibility and a legal expectation. UK guidance sets out clear prevention strategies designed to protect patient wellbeing and reduce avoidable harm.
When prevention measures are applied consistently, the risk of pressure sores can be significantly reduced. When they are not, the consequences for the individual can be serious and long lasting.
External guidance: NHS guidance on pressure sores
Monitoring and escalation
Ongoing monitoring is essential in any care setting. When early signs of pressure damage are identified, care plans should be reviewed and concerns escalated promptly.
Failure to act on early indicators can allow minor skin damage to progress into more serious injuries that are difficult to treat and slow to heal.
This article is for general information only and does not provide medical advice.