
Pressure sores, also referred to as pressure ulcers or bedsores, are injuries to the skin and underlying tissue that develop when pressure restricts blood flow to an area of the body for a prolonged period. They are most commonly associated with people who have limited mobility and are frequently seen in hospitals, care homes, and community care settings across the UK.
Although pressure sores can develop quickly, many are widely regarded as avoidable when appropriate care standards are followed. For this reason, their presence often raises important questions about whether risk was recognised early enough and whether reasonable preventative steps were taken.
What are pressure sores
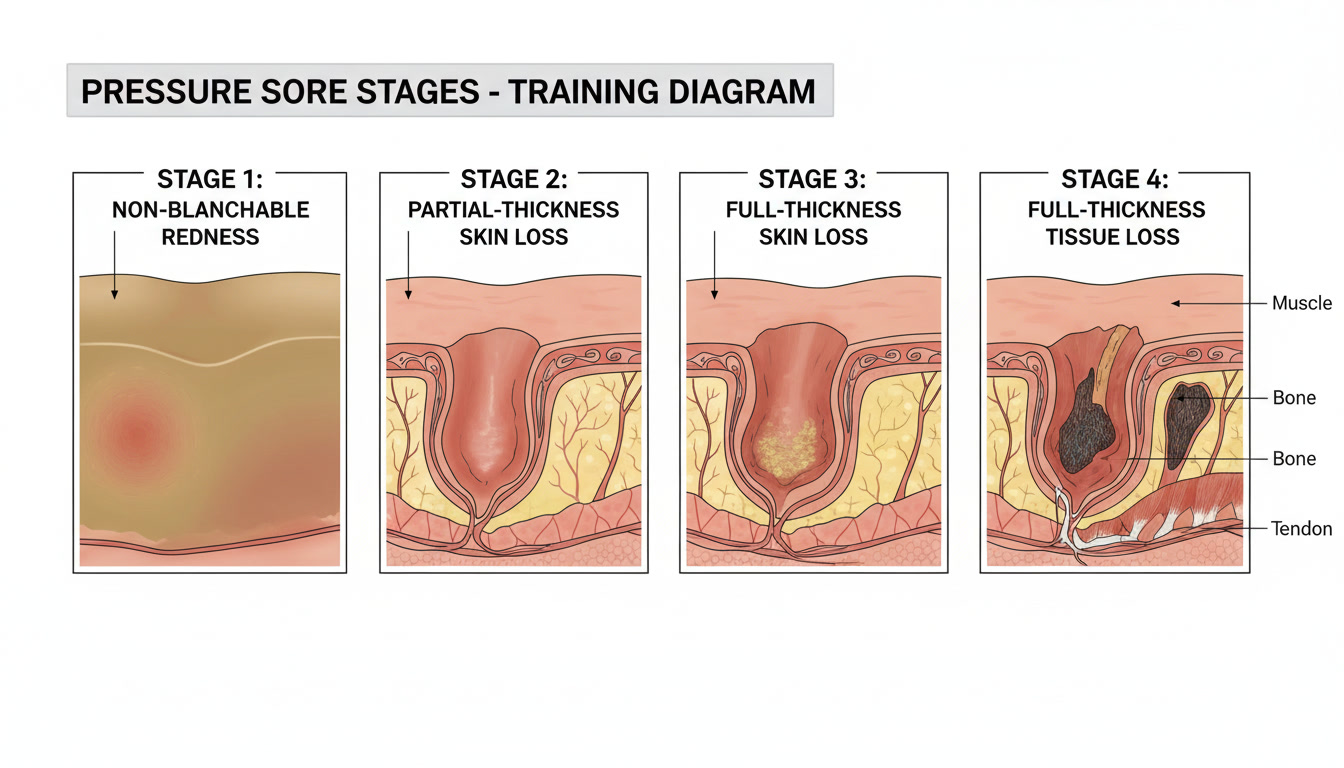
Pressure sores occur when constant pressure, or pressure combined with friction or shear, reduces blood supply to the skin. Without sufficient oxygen and nutrients, the affected tissue becomes damaged and begins to break down. Over time, this can lead to open wounds that are slow to heal and vulnerable to infection.
They typically develop over bony areas of the body such as the heels, ankles, hips, tailbone, elbows, and shoulder blades. Moisture from sweating or incontinence, along with poor nutrition or dehydration, can increase the risk further.
Who is most at risk
Some individuals are more vulnerable to pressure sores due to reduced mobility or underlying health conditions. Identifying these risks early is a core part of safe care planning.
- People who are confined to bed or a chair for long periods
- Older adults with reduced skin elasticity
- Individuals recovering from surgery or serious illness
- People receiving long term residential or nursing care
- Those who rely on others for movement or repositioning
Expected standards of care
Care standards in the UK place a clear responsibility on providers to assess pressure sore risk and take reasonable steps to prevent harm. This responsibility applies across hospitals, care homes, and community care environments.
Preventative measures typically include regular risk assessments, planned repositioning schedules, routine skin inspections, use of pressure relieving mattresses or cushions, and attention to hydration and nutrition. These steps are widely recognised as basic components of safe care.
When care standards fail
Care standards may be considered to have failed when pressure sores develop despite clear risk factors being present and not adequately managed. This may involve missed or delayed risk assessments, inconsistent repositioning, lack of monitoring, or incomplete record keeping.
In many cases, the issue is not a single error but a pattern of omissions over time. Reviewing care plans and daily records can help establish whether preventative steps were planned, carried out, and reviewed as required.
Further information
More detailed information about pressure sores, prevention responsibilities, and how care standards are assessed in a legal context
is available on the Curtis Legal pressure sores information page:
Pressure sores and care standards
This article is for general information only and does not provide medical advice.